What it's like to treat depression with ketamine
Sophie Saint Thomas, a 31-year-old writer in Brooklyn, developed PTSD and depression after a series of traumatic incidents in her life. Typical medications didn’t make a significant difference in her mental health, so her psychiatrist recommended she try ketamine infusions. Ketamine is a drug that’s been used in medical settings as an anesthetic for decades (and as a party drug for just as long) but lately, there's been a lot of buzz about how ketamine can treat depression. For the latter, patients typically receive regular IV infusions of the drug under a doctor’s supervision over several weeks or months.
The treatment transformed Saint Thomas’s quality of life. “I started to feel a lot better about halfway through and was out of the depressive hole by the sixth session,” she says. “While previously I could get sucked into a black hole of depression that included suicidal ideation, the infusions brought me back to a stable baseline. It really changed everything for me. I felt like myself again and got my confidence back.”
Anecdotally, ketamine holds a lot of promise for treating severe depression and other conditions like PTSD, though the research on its efficacy and safety is still developing. Here’s what we know so far about ketamine’s use as a mental health therapy.
How does ketamine work?
Ketamine is considered a psychedelic because it can induce hallucinations, as well as profound insights and feelings of euphoria and relaxation. It’s also a dissociative drug, meaning that it makes people feel disconnected from their bodies and surroundings.
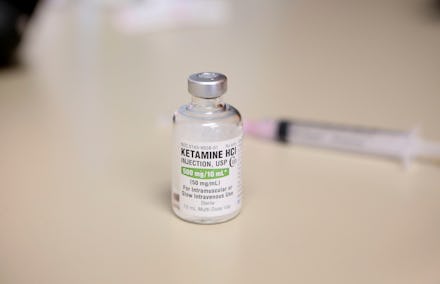
Patients who receive ketamine as a treatment for depression typically get it via IV, a process that takes about an hour, says Dr. David Mahjoubi, owner of Ketamine Healing Clinic of Los Angeles and anesthesiologist at Cedars-Sinai Medical Center in Los Angeles. People usually get five or six infusions over two weeks and then take “maintenance doses” once a month to once a year, depending on their needs. Mahjoubi provides patients with blindfolds and noise-blocking headphones to help them focus in on the experience.
What is it ketamine's link to depression?
Almost 70 percent of patients given ketamine for treatment-resistant depression report that it helps, says anesthesiologist Dr. Bill Code, who administers ketamine to treat depression and chronic pain in his practice and is on the regional advisory committee of Royal College of Physicians and Surgeons of Canada. Ketamine is believed to increase transmission of the crucial neurotransmitter glutamate in the brain, Code explains. It also may help synapses — the points of connection between brain cells — regrow.
“The modern concept of depression is reduced brain connections often precipitated by major stress and cortisol production within the body,” Code says. So, restoring those connections may be key to alleviating depression. Similar to what Saint Thomas experienced, ketamine researchers have described it as “stabilizing the brain in a well state.” Ketamine also activates the opiate receptors, which could lead to anxiety reduction, Mahjoubi says.
It’s very fast-acting, he says, so people usually see improvements in their mental health within a few days or weeks. SSRIs, a popular antidepressant class that include Prozac, take weeks to activate your G-proteins — chemical switches that transmit signals from outside stimuli to inside brain cells — while ketamine can take minutes, says Dr. John Huber, a forensic psychologist who has overseen ketamine trials. “People with large numbers of G-proteins report being depressed,” he explains.
On the psychological level, Ketamine has a number of effects that can lead to alleviation of depression, including meaningful realizations, decreased anxiety and negative thinking, increased energy, and easier processing of past trauma, says Mahjoubi. He describes it as a “deep therapy session with oneself.”
What are the risks?
When used recreationally, without the ability to carefully control the dose or be sure that there’s nothing else mixed in with the drug, ketamine can cause cognitive impairment, an inability to control your body known as a “K-hole,” and, in the case of severe overdose, respiratory and cardiac problems. If abused repeatedly, it can lead to bladder and kidney issues. If ketamine is used under the supervision of a doctor, the risks are lower, says Mahjoubi. He sometimes sees people experience nausea or headaches, which he treats with anti-nausea and anti-headache medication.
Ketamine use needs to be carefully supervised because it can increase blood pressure in the heart and brain, says Dr. Soyona Rafatjah, medical director and co-founder at the primary care and integrative medicine private practice PrimeHealth. “There is potential for overdosing when used recreationally,” she says. “Therefore, it should be used therapeutically with great caution in those with increased risk of substance abuse.”
Saint Thomas remembers feeling woozy and says she wouldn’t drive after getting a ketamine infusion. Otherwise, though, “the infusions themselves are fun,” she says. Fortunately, she experienced a calmer and more improved mood without any major side effects.
Is it legal?
While recreational use of ketamine is illegal, as the FDA deems it a schedule III substance, it is legal for doctors to administer it to patients in a clinical setting. It hasn’t yet made it to the mainstream, but there are several ketamine clinics throughout the country. Ketamine IV infusions are an “off-label” treatment, which means the FDA hasn’t approved them, but they’re not forbidden either, Code explains.
There’s another ketamine treatment that gained FDA approval for alleviating treatment-resistant depression in March. It’s a prescription nasal spray containing a form of ketamine called esketamine that is meant to be used only at a doctor’s office or clinic. However, since this method is very new, most ketamine clinics are using IVs to administer the drug, says Code.
If you’re interested in using ketamine for depression, Code advises looking for a qualified physician who has experience with ketamine therapy. Make sure the clinician knows about your medication use and psychiatric history so that they can minimize the treatment’s risks.